Advanced nanofibrous membranes can tackle diabetic wounds with precision
Diabetic wounds are notoriously challenging to treat, due to prolonged inflammation and a high risk of infection. Traditional treatments generally offer only passive protection and fail to dynamically interact with the wound environment.
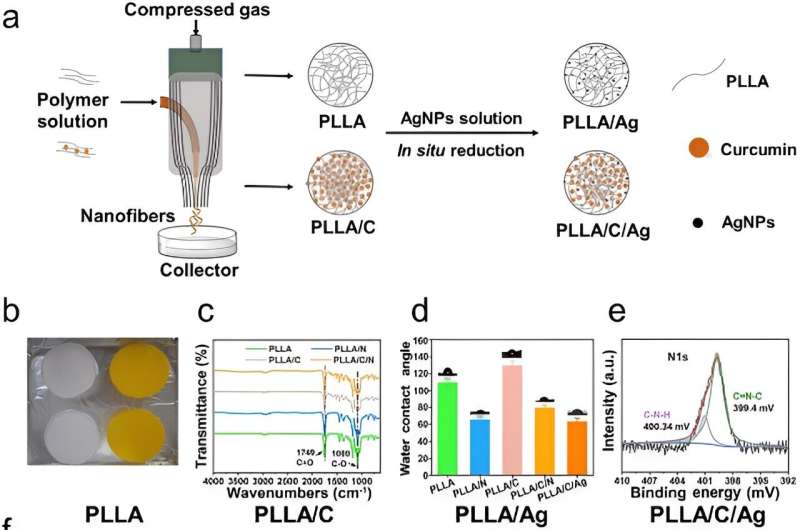
The creation of bioactive dressings such as poly (L-lactic acid) (PLLA) nanofibrous membranes incorporated with AgNPs and curcumin (PLLA/C/Ag) membranes signifies a crucial shift towards therapies that actively correct imbalances in the wound healing process, offering a more effective solution for managing diabetic wounds.
In a new article in Burns & Trauma on June 5, 2024, a research team from Mudanjiang Medical University and allied institutions assesses the effectiveness of PLLA nanofibrous membranes.
Infused with curcumin and silver nanoparticles, these membranes are designed to substantially enhance the healing processes in diabetic wounds by targeting fundamental issues like excessive inflammation and infection.
This research centered on developing PLLA/C/Ag nanofibrous membranes through air-jet spinning, achieving a consistent fiber distribution essential for effective therapeutic delivery. The membranes boast dual benefits: antioxidant properties that reduce harmful reactive oxygen species in wound environments and potent antibacterial activity that decreases infection risks.
In vivo tests on diabetic mice demonstrated the membranes' capability to promote crucial healing processes such as angiogenesis and collagen deposition. These findings illustrate that PLLA/C/Ag membranes not only protect wounds but also actively support and expedite the healing process, marking them as a significant therapeutic innovation for diabetic wound management with potential for broader chronic wound care applications.
Dr. Yanhui Chu, a principal investigator of the study, states, "The PLLA/C/Ag membranes are a significant breakthrough in diabetic wound care. Their ability to effectively modulate the wound environment and enhance healing could establish a new standard in treatment, providing hope to millions affected by diabetes-related complications."
The deployment of PLLA/C/Ag nanofibrous membranes in clinical environments could transform the treatment of diabetic wounds, offering a more active and effective approach. Beyond diabetes management, this technology has the potential for extensive applications in various chronic wounds, paving the way for future breakthroughs in bioactive wound dressings.
This study not only progresses our understanding of wound management but also paves new paths for developing adaptive treatments for complex wound scenarios.
More information: Yan Wu et al, Immunomodulatory poly(L-lactic acid) nanofibrous membranes promote diabetic wound healing by inhibiting inflammation, oxidation and bacterial infection, Burns & Trauma (2024).
Provided by TranSpread
















